Exploring the biopsychosocial impact of recalcitrant eczema - a case report
DOI:
https://doi.org/10.33178/SMJ.2025.1.18Keywords:
biopsychosocial model, Dermatology, EczemaAbstract
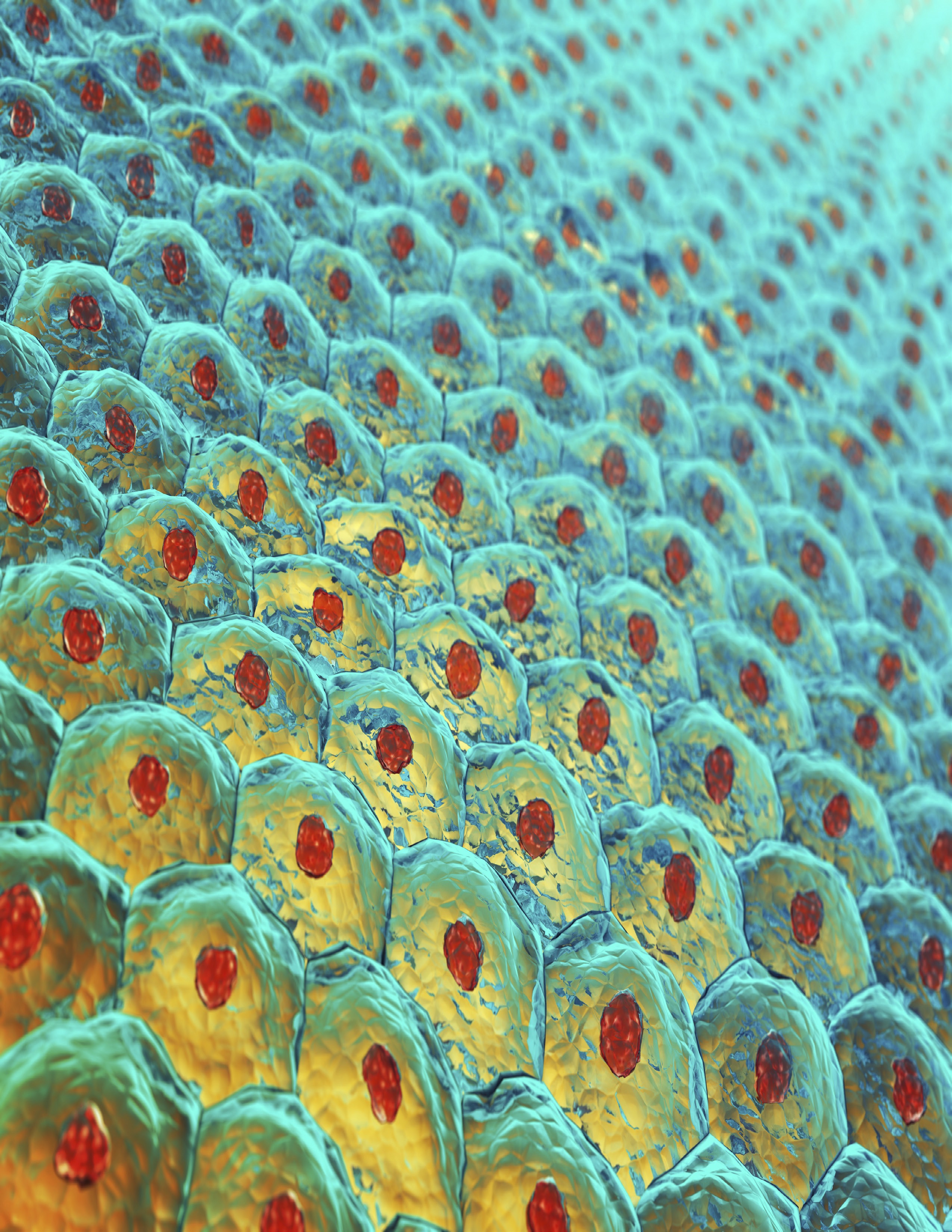
Introduction: A 13-year-old female patient presents with a complex case of severe eczema ongoing for over a year. This case report integrates the biopsychosocial model, focusing on the biological, psychological, and social determinants affecting flare onset and guiding the treatment plan.
Methods: Consent was obtained from the patient and her mother. A comprehensive review of the patient's medical file, including past medical and surgical history, family, and social history was conducted. A multidisciplinary approach drawing on opinions from dermatology, primary care, and social work, was used to optimize treatment.
Results: Through a biological perspective, the patient has widespread excoriation and lichenification throughout the body, likely attributed to hormonal changes associated with menarche and family history. Psychologically, the patient described a shift from her previously calm demeanor to a more agitated and anxious state. Socially, the patient reports social withdrawal and the stigma associated with her flares.
Discussion: This case highlights the importance of incorporating the biopsychosocial model when treating severe and relapsing cases of eczema in pediatric populations. Dealing with chronic, worsening flares, as reported in the case, highlights the vital need for a multidisciplinary approach to address the emotional and physical impacts.
Conclusion: The patient's case represents a common pediatric presentation in general practice and illustrates the necessity of incorporating the biopsychosocial model when addressing treatment options for chronic skin conditions such as eczema.
References
Borrell-Carrio F. The biopsychosocial model 25 years later: Principles, practice, and scientific inquiry. The Annals of Family Medicine. 2004;2(6):576-582. doi:10.1370/afm.245
Johnson YL, Woodward K, Dampier C, et al. Biopsychosocial factors associated with parenting stress in pediatric sickle cell disease. J Clin Psychol Med Settings. 2022;29:365–74. doi:10.1007/s10880-021-09837-6
Rey R, Duggan E, O’Connor C. Accuracy and confidence of Irish general practitioners in diagnosing skin disease in patients with darkly pigmented skin. Skin Health and Disease. 2024;4(6). doi:10.1002/ski2.465
Biagini Myers JM, Khurana Hershey GK. Eczema in Early Life: Genetics, the Skin Barrier, and Lessons Learned from Birth Cohort Studies. The Journal of Pediatrics. 2010;157(5):704-714. doi:https://doi.org/10.1016/j.jpeds.2010.07.009
Weare-Regales N, Chiarella SE, Cardet JC, Prakash YS, Lockey RF. Hormonal Effects on Asthma, Rhinitis, andEczema. The Journal of Allergy and Clinical Immunology: In Practice. 2022;10(8):2066-2073. doi:https://doi.org/10.1016/j.jaip.2022.04.002
Brunner PM, Guttman-Yassky E, Leung DYM. The immunology of atopic dermatitis and its reversibility with broad-spectrum and targeted therapies. Journal of Allergy and Clinical Immunology. 2017;139(4):S65-S76. doi:https://doi.org/10.1016/j.jaci.2017.01.011
Shah N, Alhusayen R, Walsh S, Shear NH. Methotrexate in the Treatment of Moderate to Severe Atopic Dermatitis: A Retrospective Study. Journal of Cutaneous Medicine and Surgery. 2018;22(5):484-487. doi:https://doi.org/10.1177/120347541878133
Bawany, F., Northcott, C. A., Beck, L. A., & Pigeon, W. R. (2021, April). Sleep disturbances and atopic dermatitis: Relationships, methods for assessment, and therapies. The journal of allergy and clinical immunology. In practice. https://pmc.ncbi.nlm.nih.gov/articles/PMC9026738/#:~:text=Increased%20disease%20severity%20as%20measured,0001)
Schonmann, Y., Mansfield, K. E., Hayes, J. F., Abuabara, K., Roberts, A., Smeeth, L., & Langan, S. M. (2020, January). Atopic eczema in adulthood and risk of depression and anxiety: A population-based Cohort Study. The journal of allergy and clinical immunology. In practice. https://pmc.ncbi.nlm.nih.gov/articles/PMC6947493/#bib26
Sutin, A. R., Zonderman, A. B., Ferrucci, L., & Terracciano, A. (2013, November). Personality traits and chronic disease: Implications for adult personality development. The journals of gerontology. Series B, Psychological sciences and social sciences. https://pmc.ncbi.nlm.nih.gov/articles/PMC3805287/
Harter K, Hammel G, Kirchberger I, Traidl-Hoffmann C. Social and psychosocial effects on atopic eczema symptom severity – a scoping review of observational studies published from 1989 – 2019. Journal of the European Academy of Dermatology and Venereology. 2020;35(4). doi:https://doi.org/10.1111/jdv.16950
Courtney A, Su JC. The Psychology of Atopic Dermatitis. Journal of Clinical Medicine. 2024;13(6):1602. doi:https://doi.org/10.3390/jcm13061602
Dalgard FJ, Bewley A, Evers AW, et al. Stigmatisation and body image impairment in dermatological patients: protocol for an observational multicentre study in 16 European countries. BMJ Open. 2018;8(12):e024877. doi:https://doi.org/10.1136/bmjopen-2018-024877
Downloads
Published
License
Copyright (c) 2025 Dermatology Society, Ghufran Bander, Alexander Johnson, Nora Skurdina, Maheen Junaid

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.